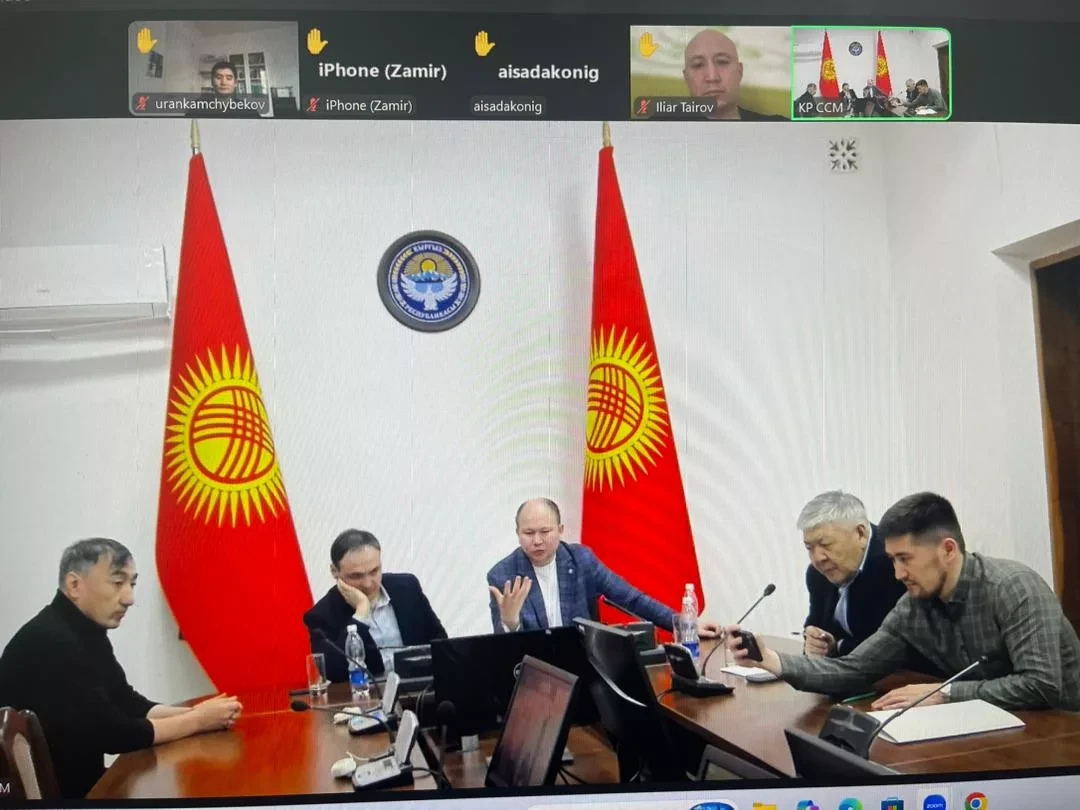
- Currently, Askerov heads the Scientific Center for Maternal and Child Health named after A. Tashieva.
In his speech, he emphasized that medical education in these areas is undergoing changes due to the introduction of new technologies and a shift towards a competency-based training model. Simulation training, the development of narrow specialties, and the strengthening of clinical practice play a special role in this process; however, effective implementation requires systemic investments in educational infrastructure.
Quote:
“With the rapid development of medical knowledge and technologies, educational programs are becoming increasingly complex, and creating effective education in obstetrics, gynecology, and pediatrics that can prepare future specialists in a short time is a global challenge. In our country, programs in these areas strive for standardization by integrating key competencies; however, early clinical practice remains overlooked.
In the fields of obstetrics, gynecology, and pediatrics, there is a transition to competency-based medical education (CBME), where the focus is on developing surgical skills and diagnostic competence, rather than just years of experience. Modern programs actively utilize simulation training, virtual reality, and specialized internships (for example, in perinatal medicine, pediatric gynecology, and reproductive medicine), which contribute to the formation of independent clinical competence.
The American Board of Obstetrics and Gynecology (ABOG) recognizes a number of narrow specialties such as perinatal medicine, reproductive endocrinology, gynecologic oncology, and female pelvic medicine.
In the process of in-depth training, the emphasis is placed on modeling surgical skills (for example, laparoscopy, hysteroscopy) and managing emergency obstetric situations, which significantly increases the confidence of trainees. New continuing education programs are emerging that cover reproductive health management at all stages of life.
However, there is insufficient depth of training in this direction, which includes three years of general residency and three-year internships (for example, in pediatric cardiology or neonatology). The general practice program in the first year of training addresses more issues of therapy and family medicine; however, clinical bases for family medicine leave much to be desired.
There are also unresolved issues in the transition from theoretical training to clinical internships and continuous professional development. For example, specializations such as managing high-risk pregnancies and complex gynecological surgeries remain underdeveloped.
Overall, education in obstetrics, gynecology, and pediatrics is in a state of transformation, accompanied by the introduction of technologies and standardization; however, significant differences remain, especially in resource-limited settings.
It is important to note that training in adequate clinical conditions can help identify residents who need additional support and ensure a broader skill set by the end of their training. Educational sessions in emergency obstetric care clinics (for example, for postpartum hemorrhage or shoulder dystocia) are often not conducted in interdisciplinary groups, which reduces effectiveness. Research shows that team simulation training improves both technical skills and communication, which is critically important for patient safety.
Modeling surgical skills also plays a key role in training obstetricians and gynecologists. Due to limited working hours and safety considerations, residents have insufficient opportunities to practice complex surgeries on patients. For this, simulations using anatomical models and virtual simulators are employed.
Although scenarios of normal childbirth are already practiced in simulations, critical situations such as cesarean sections due to obstructed labor or amniotic fluid embolism are not included in training programs. This highlights the need for the development of simulation training with a focus on rare but critically important situations to prepare graduates for emergency conditions.
Modern advancements in obstetrics and gynecology, such as new surgical techniques and medications, require physicians to continuously update their knowledge and skills. Continuing education is not limited to lectures and reading literature; experienced specialists increasingly use simulation methods, especially in emergency obstetric situations.
Many medical institutions now conduct regular drills, involving interns, physicians, nurses, and other staff. These events promote continuous learning and strengthen teamwork. Studies show that even basic simulations combined with e-learning can significantly enhance the knowledge and skills of medical students and nurses.
In settings with developed infrastructure, simulation training programs show a reduction in the number of lawsuits and adverse events in obstetric-gynecological and pediatric practice. However, challenges in scaling these methods remain, requiring attention to issues of cost and accuracy of simulations. The growing interest in virtual and augmented reality, as well as artificial intelligence in education, is promising but requires careful evaluation.
Thus, investments in educational infrastructure and the adaptation of training programs are critical for preparing specialists. Modern educational strategies focus on practical skills and validated competencies, using simulations and technologies to train physicians who possess both technical skills and an understanding of the humanistic aspects of women's and children's health.”